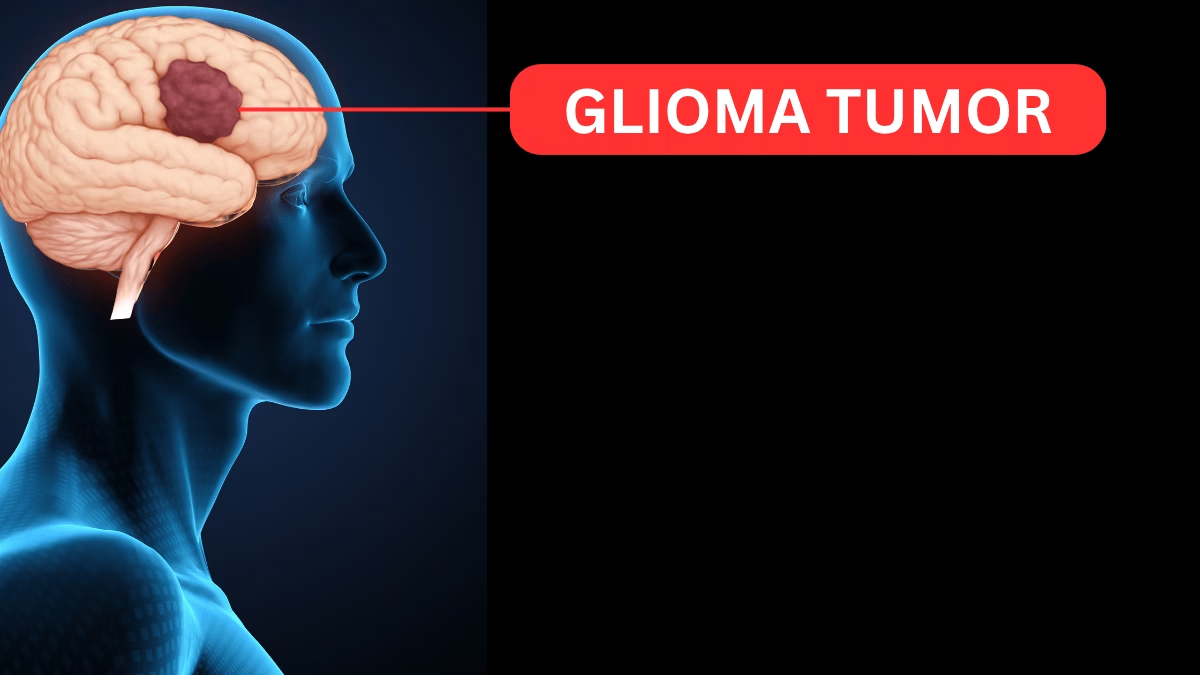
Glioma is not just one disease—it’s a broad class of primary tumors that arise from glial cells in the brain or spinal cord. These tumors can vary tremendously in behavior, aggressiveness, symptoms, and outcomes. Here is a detailed, up-to-date, and expert-backed overview of glioma from origin and classification to diagnosis, treatment, and prognosis.
What Is a Glioma?
Glial cells—the support cells of the nervous system—include astrocytes, oligodendrocytes, and ependymal cells. When these cells grow uncontrollably, they form a glioma. Gliomas account for about 30% of all brain tumors and 80% of malignant brain tumors in adults.
ALSO READ : The Courageous Battle: Confronting Central Nervous System Glioma
Types of Glioma
Gliomas are classified based on the glial cell type from which they originate:
- Astrocytoma: Develops from star-shaped astrocytes. Grades range from pilocytic astrocytoma (I, usually benign) to glioblastoma multiforme (IV, most aggressive).
- Oligodendroglioma: Arises from oligodendrocytes. Usually slow-growing but can become more aggressive.
- Ependymoma: Originates from ependymal cells that line the ventricles and central cord.
- Mixed Gliomas (Oligoastrocytoma): Contain more than one glial cell type.
- Diffuse Midline Glioma: A subtype, often occurring in children, that is highly aggressive and difficult to treat, especially when affecting the brainstem or spinal cord.
Causes and Risk Factors
- Genetic mutations: Most gliomas start after spontaneous mutations in genes regulating cell growth.
- Radiation exposure: Previous radiation therapy (especially to the head) increases risk.
- Age: Can occur at any age, but most common in adults between 45–65.
- Family history: Rarely, genetic syndromes (like neurofibromatosis) can increase the risk.
Symptoms
Symptoms depend on tumor size, growth rate, and location in the brain or spinal cord:
- Persistent or worsening headaches
- Seizures
- Changes in memory, personality, or cognition
- Vision or speech disturbances
- Weakness, numbness, or loss of function on one side of the body
- Difficulties with walking or balance
- Nausea or vomiting
Diagnosis
Diagnosing glioma requires a combination of clinical evaluation and advanced imaging:
- Neurological examination: Assesses cognition, movement, reflexes, and senses.
- Imaging: MRI is the gold standard; CT may also be used.
- Biopsy: Surgical removal of a small tumor sample for pathological analysis. Determines exact type and grade.
- Molecular/genetic testing: Identifies mutations or biomarkers (like IDH1, 1p/19q codeletion, H3 K27M) that influence diagnosis and treatment.
WHO Classification and Grading (2021–2025 Updates)
The World Health Organization (WHO) classifies gliomas from grade I to IV:
| Grade | Description | Typical Tumors | Behavior |
|---|---|---|---|
| I | Least aggressive | Pilocytic astrocytoma | Often curable |
| II | Low-grade, slow-growing | Diffuse astrocytoma, oligodendroglioma | Can recur/progress |
| III | Anaplastic, malignant | Anaplastic astrocytoma | Aggressive, recurring |
| IV | Most aggressive, rapidly growing | Glioblastoma multiforme, diffuse midline glioma | Poor prognosis |
Recent updates include a molecular classification that helps tailor treatments and prognosis more precisely.
Treatment
Management is individualized, considering tumor location, grade, patient health, and genetic features:
1. Surgery:
When possible, surgical resection is the first step—aiming to remove as much tumor as safely possible.
2. Radiation Therapy:
Often follows surgery, especially for high-grade or inoperable tumors.
3. Chemotherapy:
Temozolomide is standard for glioblastoma and some other gliomas. Other agents or clinical trials may be used.
4. Targeted and Immunotherapies:
Newer approaches target specific genetic mutations or harness the immune system (e.g., checkpoint inhibitors, tumor vaccines).
5. Supportive care:
Steroids (to reduce swelling), antiepileptic drugs (for seizures), and therapies for cognitive or physical support.
6. Palliative care:
Essential for high-grade gliomas to optimize quality of life when cure isn’t possible.
Prognosis
Outcome varies widely. Key factors include tumor type, grade, genetic markers, patient age, and overall health.
- Low-grade glioma (grade I–II): Median survival can exceed 10 years, especially with complete surgical removal.
- High-grade glioma (grade III–IV, e.g., glioblastoma): Median survival difficult to exceed 16–18 months with standard care, although newer targeted and experimental therapies offer hope for select patients.
- Diffuse midline glioma: Especially poor outlook, with most patients surviving less than a year.
Quality of Life and Coping
- Cognitive, emotional, and physical challenges are common.
- Rehabilitation, support groups, and neuro-oncology specialists are key for maintaining quality of life and addressing symptoms proactively.
Research and Future Directions
- Precision medicine: Tumor genetics now drive many therapy decisions.
- Clinical trials: New drugs, immunotherapies, gene therapies, and advanced radiotherapy are active research areas.
- Liquid biopsy: Blood or spinal fluid tests may soon help diagnose and monitor glioma progression non-invasively.
When to See a Doctor
Anyone experiencing persistent headaches, unexplained neurological symptoms, or new seizures—especially with risk factors—should seek prompt medical attention for evaluation.
Conclusion:
Glioma is a complex group of brain tumors that vary from curable, slow-growing forms to extremely aggressive cancers like glioblastoma. Early diagnosis, refined treatment (often in major neuro-oncology centers), and supportive care are vital. Research is evolving rapidly, offering new hope for personalized and effective therapies in the future. If you or a loved one is facing a glioma diagnosis, consult with a multidisciplinary team to explore all evidence-backed options and clinical trials, and seek support for both physical and emotional needs.
Disclaimer:
The information provided in this content is for educational and informational purposes only and does not constitute medical advice. It is not a substitute for professional diagnosis, treatment, or consultation with a qualified healthcare provider. Always seek the advice of your physician or other qualified health professional with any questions you may have regarding a medical condition. The author and publisher disclaim any liability for decisions made based on this information.